In support of health system resilience: Researchers highlight the role of primary care during the pandemic in Ontario

A team led by researchers from the Department of Family and Community Medicine at the University of Toronto has authored a three-part brief on the strengths and challenges of primary care (part 1, part 2 and part 3) in the pandemic for the Ontario COVID-19 Science Advisory Table. The reports, published on Oct. 3, 2022, detail the work of primary care providers during the first two years of the pandemic, outline issues affecting primary care in Ontario, and offer lessons learned to improve access to primary care.
“The pandemic is not over, and COVID-19 is increasingly an illness that will be managed in the community, supported by family doctors, nurse practitioners and primary care teams. The Science Table wanted to understand the evidence base around the contributions of primary care to the pandemic response so far, as well as current strengths and challenges that will affect response to future waves. At this time it is critical to understand the lessons learned from the last two and a half years ,” says Dr. Danielle Martin, Professor and Chair of the Department of Family and Community Medicine at U of T, who conceived the briefs.
The core authors include experts in primary care from across Ontario with a wide variety of backgrounds, including Drs. Imaan Bayoumi, Azza Eissa, Noah Ivers, Tara Kiran, Derelie Mangin, Sarah Newbery, Andrew Pinto and Kamila Premji. The team analyzed more than 200 articles for the research and consulted experts broadly in its work.
The release of the briefs is the last official act of the Ontario COVID-19 Science Advisory Table. Comprised of scientific experts and health system leaders, the advisory table evaluated and reported on evidence relevant to the pandemic to guide Ontario’s response. Research shows health systems with strong primary care have better health outcomes and improved health equity at lower cost; an examination of the lessons learned about primary care in the pandemic seems a fitting capstone activity for the Science Table.
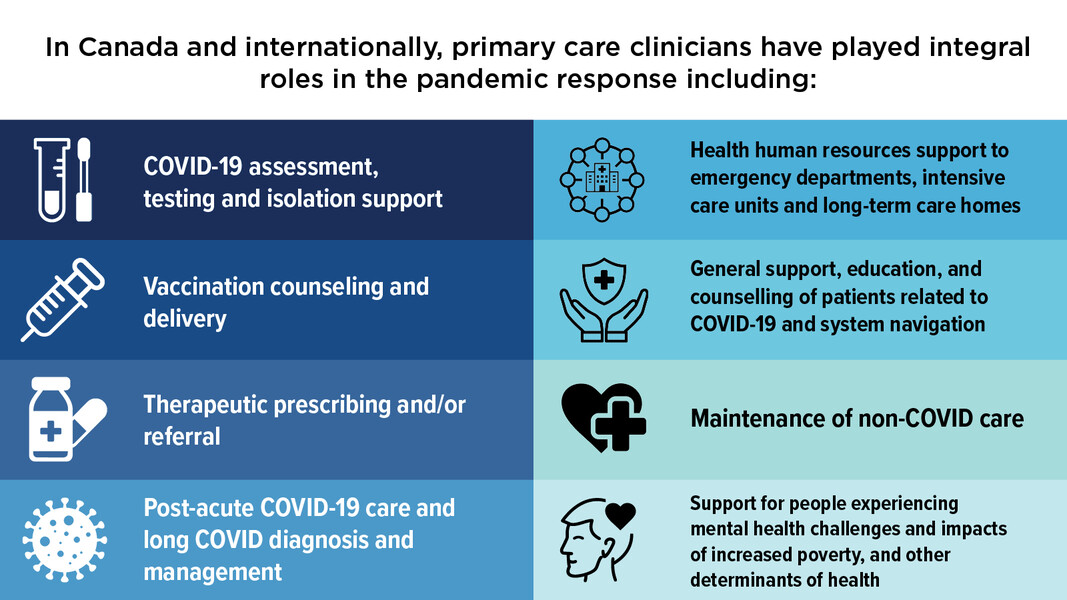
The three-part brief is an ambitious undertaking involving dozens of researchers and primary care experts from across Ontario, Canada and internationally. The briefs outline the evidence on how primary care clinicians—family doctors, nurse practitioners, pharmacists, social workers and other allied health care providers—took on new roles and worked more days to support COVID-19 care in addition to their routine clinical work, which includes preventive, chronic and acute care. Primary care clinicians in Ontario assumed new responsibilities like COVID testing, assessment and isolation; vaccine counselling and delivery; treatment prescribing and referral and post-COVID acute care. They also aided other areas of the health system like emergency departments, intensive care units and long-term care, and assisted people experiencing mental health issues as well as poverty and food insecurity.
“As misinformation rises around COVID-19, primary care clinicians are highly trusted members of their communities—they are an invaluable resource for conveying fast-changing scientific developments around prevention and treatment of COVID-19 to the public,” says Dr. Fahad Razak, scientific director of the Ontario COVID-19 Science Advisory Table and an assistant professor in the Department of Medicine at U of T.
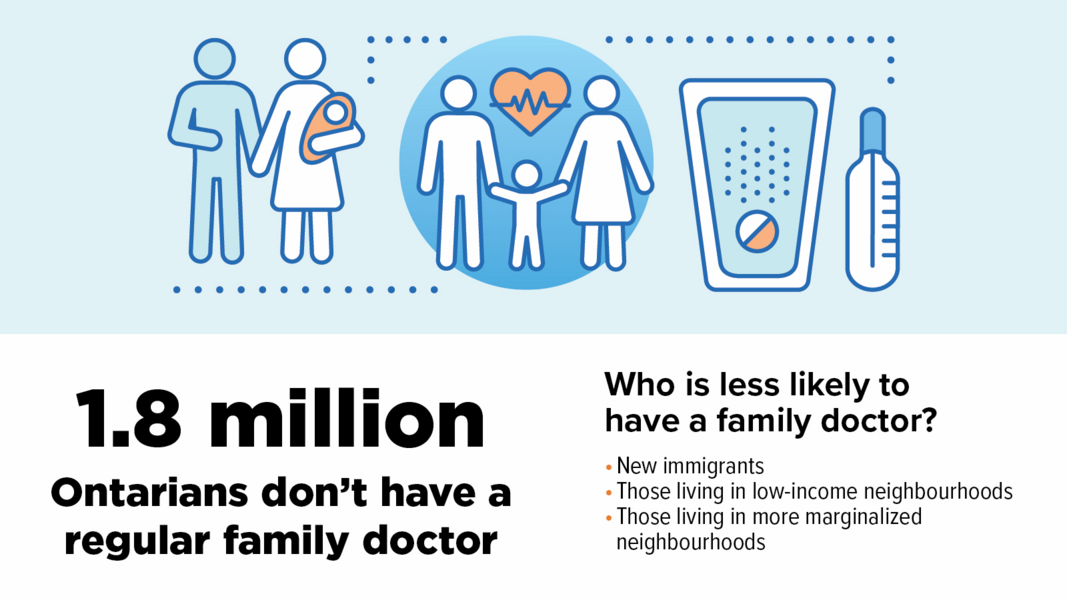
Ontario faces a significant challenge in keeping up with demand for primary care, the researchers note. About 1.8 million Ontarians do not have a regular family doctor, with new immigrants and people living on low incomes least likely to have one. Moreover, 1.7 million Ontarians have a family doctor who is of retirement age. Compounding this shortage is the decline in medical school graduates choosing to specialize in family medicine. These challenges, along with inequitable access to team-based care, shape the ability of primary care to respond to future pandemic waves and support health system recovery.
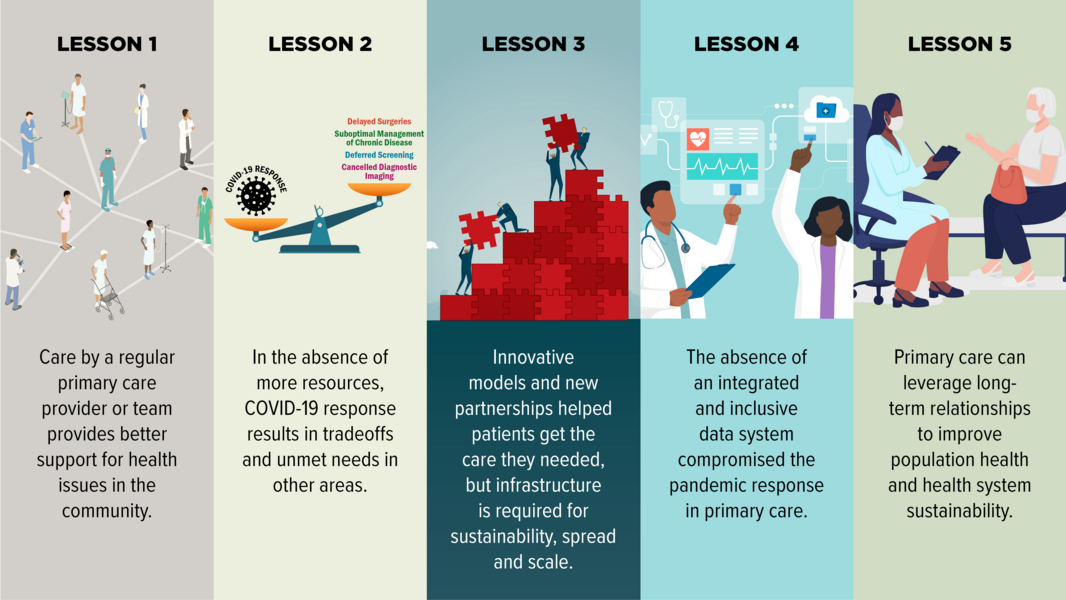
Based on their findings, the researchers outlined lessons learned:
- Care provided in formal attachment relationships and through team-based models provides superior support for COVID-19- and non-COVID-19-health issues in the community.
- In the absence of additional resources, COVID-19 response results in tradeoffs and unmet needs in other areas.
- Innovative models and new partnerships supported patients to get needed care, but infrastructure is needed for sustainability, spread, and scale.
- The absence of an integrated data system compromised the pandemic response in primary care.
- Primary care can leverage its longitudinal relationships to achieve public health aims.
Martin says the ultimate goal of the work is to provide evidence to help decisionmakers, including governments, professional associations, and front-line providers to improve the ongoing pandemic response. “We’re in a state where we’re facing significant health human resources shortages, inequitable access to teams and uncertainty about the future. My hope is that the crisis we’re facing will motivate all leaders in the system to look to the evidence about how we can best improve access to high-quality primary care for all Ontarians.”
Infographics
News



