An Online Community Space for Palliative Care Experts Forges New Connections


What are the latest trends in palliative care? How can palliative care experts apply quality improvement within their practice? How succinctly can palliative care specialists explain their stance on advance care planning?
These are some of the many questions swirling through the Division of Palliative Care online community space for faculty members at the Department of Family and Community Medicine (DFCM).
The community space began after a needs assessment found that division faculty expressed a strong desire for a sense of community among its members. There was also an expressed interest for a forum to exchange ideas and content relevant to palliative care specialists.
"There is an academic palliative care team at each of the 14 DFCM teaching sites," says Dr. Jeff Myers, Head of the Division of Palliative Care (DPC) at DFCM. "They vary substantially in size and composition, but we wanted to create opportunities to build connections between all of them. One of the ways to do that is virtually."
Using a virtual platform developed by the Canadian Partnership Against Cancer, the online space includes a repository for documents where members can read and download materials others have shared, including teaching modules, and a practice-oriented discussion forum where faculty members ask for advice and share perspectives.
"We use our online space for discussions, to seek input and to share content and ideas,” says Dr. Myers. “For example, if a discussion occurring during a Grand Rounds presentation is quite lively, we continue it on the community space and pick up some threads there."
Traffic to the virtual space continues to rise as the team ensures that the content remains relevant to members' practice. A recent focus to get members acquainted with quality improvement has proven highly successful. Following a training program hosted by Trish O'Brien and Dr. Philip Ellison of the Quality and Innovation team at DFCM, the DPC sought to maintain the learning momentum by using the community space to share scholarly articles on quality improvement.
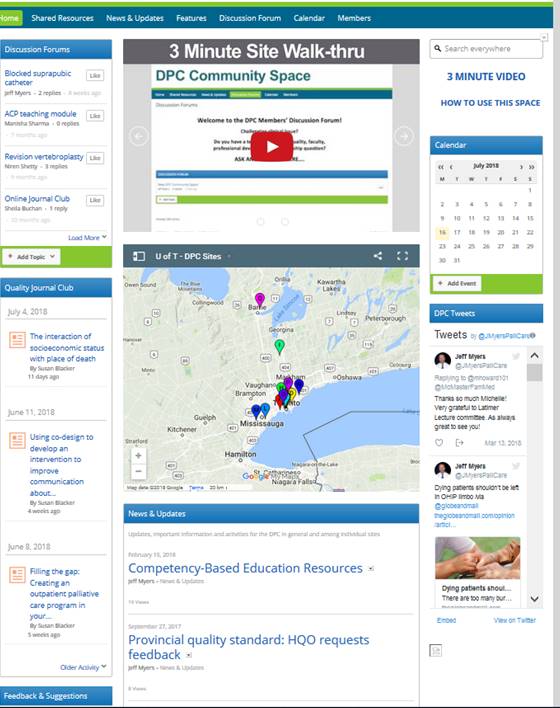
In fact, along with several offline initiatives, Susan Blacker, the DPC’s quality co-lead, has used this virtual hub for sharing articles and resources that might be well suited to supporting teams’ quality improvement work.
"I try to pick articles reflecting timely topics and quality-related themes that would lend themselves to reading and discussion at team-based journal clubs," says Susan Blacker. "We have received great feedback. Faculty members are also routinely alerted to upcoming quality improvement training sessions as well as conferences that might be interesting opportunities for presenting their work beyond our immediate division."
The online space has been particularly useful for conversations centred around topics such as advance care planning and consent, as well as the sensitive topic of medical assistance in dying (MAID) – a particularly charged subject for palliative care clinicians. Respectful discussion on the community spaced, however, allowed a consensus to be reached on a DPC position statement on MAID. On all sensitive and emerging topics, members can share resources as they evolve, discuss how it applies academically to their teaching practices, and share webinars and seminar dates. Although the conversation has only just begun, a healthy list of resources on these topics – particularly advance care planning - already exists.
Dr. Myers says that he's most excited about a new section in the community space that will address faculty and learner development and implementing competency-based education, an area where faculty communicated a need for greater guidance.
"Over the next couple of months, we are rolling out a suite of materials on assessing learners, including giving and receiving feedback, to develop a community of practice among teachers and learners,” says. Dr. Myers.
Myers hopes that the community space will be an added tool to their learning.
"We use a new term we’ve coined ‘faculty and learner development’ to replace ‘faculty development’ because we recognize the critical importance of faculty and learners working together on implementation,” says Dr. Myers. “In the same way that patients and families are now often integrated into committees and projects, our learners are integrated into all aspects of planning for competency-based education."
As it continues to grow, Dr. Myers hopes that the palliative care community space will further strengthen the sense of community among faculty members and facilitate individuals feeling more confident in their role as academic palliative care clinicians.
Related items
News