Place of Healthy Breathing: Supporting Indigenous communities during COVID-19 and beyond
Eighteen months into the COVID-19 pandemic and one year since the dehumanizing treatment and death of Joyce Echaquan, Indigenous peoples continue to experience significant disparities in the Canadian healthcare system.
On September 30, 2021, as we mark Orange Shirt Day and the first National Day for Truth and Reconciliation, University of Toronto Department of Family and Community Medicine (DFCM) faculty members are working to address the disproportionate impacts of infectious diseases on Indigenous communities and dismantle the systemic barriers that prevent Indigenous peoples from accessing care.
Toronto is home to more than 95,000 First Nations, Métis and Inuit people — the largest population of Indigenous people anywhere in the province. Of these individuals, only one in three has a primary care provider, while 38% live with two or more chronic diseases (compared to 15% of adults in Canada) and 87% live below the low-income cut off.
These statistics, alongside generations of systemic inequities and ongoing discrimination that prevent Indigenous people from accessing care, have resulted in higher rates of severe illness from COVID-19. COVID-19 hospitalization rates for Indigenous people in Toronto throughout the pandemic have been 40-80% higher than COVID-19 hospitalization rates for Toronto generally and twice as high as those for the general Ontario population.
“COVID-19 has exposed long-standing unequal distribution of health and social resources in our communities,” says Dr. Janet Smylie, DFCM’s Indigenous Health Research Lead and a Tier 1 Canada Research Chair in Indigenous Health. “We need to address these inequities in concrete, tangible ways. But to do this we need to witness and track the scale of the issues. What’s counted, counts.”
With limited resources Dr. Janet Smylie, DFCM’s Indigenous Health Research Lead and Dr. Suzanne Shoush, DFCM’s Indigenous Health Faculty Lead, have been working with community organizations to build trust in the health system, support COVID-19 testing and vaccination and collect data to inform research and policy changes.
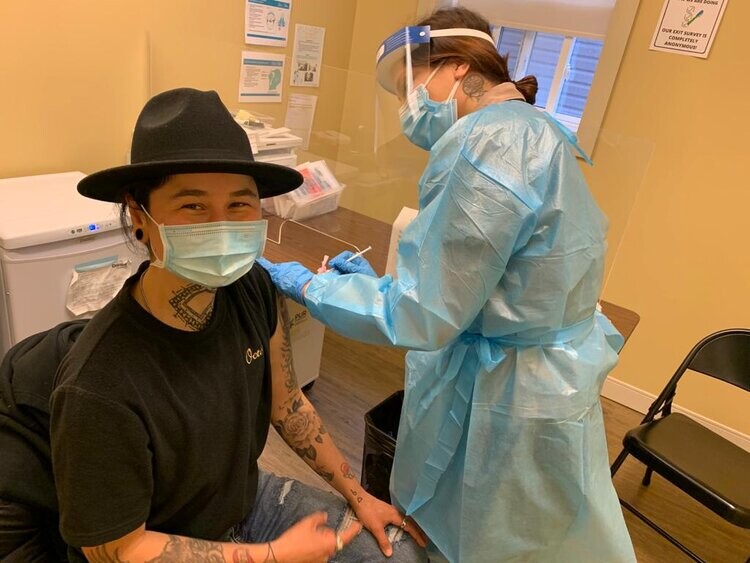
The Auduzhe Mino Nesewinong COVID-19 clinic opened in October 2020 to provide integrated testing and case management, contact tracing, outreach supports and referrals. The Indigenous community-led centre is a collaboration between Na-Me-Res, Seventh Generation Midwives Toronto, Well Living House at St. Michael’s Hospital and the Centre for Wise Practices in Indigenous Health at Women’s College Hospital.
Meaning “Place of Healthy Breathing” in the Anishinaabe language, the Auduzhe Mino Nesewinong team has conducted more than 1,100 COVID-19 tests and administered over 6,800 COVID-19 vaccinations at Auduzhe and partnered clinics.
“We knew at the beginning of the pandemic that there was dire need to have a for-Indigenous by-Indigenous comprehensive COVID-19 response,” says said Steve Teekens, Executive Director of Na-Me-Res, an emergency shelter and housing organization. “Our team has been able to provide culturally safe services in a warm inviting space, while providing quality services to our community members.”
Auduzhe Mino Nesewinong runs in tandem to We Count COVID-19, an Indigenous community-owned database about First Nations, Inuit and Métis COVID-19 spread led by Dr. Smylie, who is also the Director of Well Living House.
“Community is the foundation of both the clinic and our research,” says Dr. Smylie. “The clinic is a critical part of the COVID-19 response. But looking ahead, we need the research component to challenge the policies that have led us to this point and make lasting change. The two go hand-in-hand.”
Given historic and ongoing abuse and discrimination that Indigenous peoples experience within the Canadian health system, creating safe spaces with trusted partners has been key.
“The importance of this project is profound, in particular because it is a combination of service and research that is community-led. All systems are informed by the urban Indigenous community and designed specifically for that community – and the outreach and supports are based on Indigenous kinship systems of inclusion, care and self-determination,” Cheryllee Bourgeois, Exemption Métis Midwife at Seventh Generation Midwives Toronto told Women’s College Hospital.
“To date, 50% of Toronto’s First Nations, Métis and Inuit population has had two doses of a COVID-19 vaccine. Leaving 50% vulnerable to the disease,” says Dr. Smylie. “Some days feel overwhelming but other days I feel hugely optimistic, especially when I see colleagues across DFCM stepping up to staff our swabbing and vaccination clinics.”
Beyond COVID-19 and throughout the Canadian healthcare system, there is significant work needed to eradicate anti-Indigenous discrimination, work that we are all accountable for.
As Dr. Smylie and colleagues wrote in the Globe and Mail last year, “We need to recognize and fight [anti-Indigenous discrimination in hospitals] the same way we do infection. We need leaders who label it as a preventable and life-threatening organizational challenge, and who promote cross-system extermination, ongoing vigilance and prevention. We need action, including co-ordinated systems-level responses that hold individuals and institutions accountable.”
News