#TeamVaccine: All Toronto LTC homes vaccinated ahead of schedule thanks to primary care teams
Image: Together as #TeamVaccine, DFCM faculty Drs. Karen Tu (University Health Network - Toronto Western), Karen Weyman (Unity Health, St. Michaels), Leslie Beyers (Sunnybrook Health Sciences Centre), Karen Fleming (Sunnybrook Health Sciences Centre) and Rachel Peters (University Health Network – Toronto Western) with Dr. Peter Derkach (West Park Healthcare Centre).
In the race to protect Toronto’s most vulnerable populations from COVID-19, primary care providers have pulled together to vaccinate all 87 Toronto long-term care homesahead of schedule.
When the province set a target of vaccinated all eligible long-term care residents by Jan 21, there was little the next big question was, how?
This is a massive undertaking with complicated logistics. Dubbed #TeamVaccine, family doctors, nurses, pharmacists and other primary care providers are sharing resources and expertise to administer the first vaccine doses quickly and safely.
That meant vaccinating two or three long-term care homes each day. A feat made possible thanks to incredible leadership and collaboration between Toronto’s health networks and staff working in long-term care settings.
Dr. Camille Lemieux, an Associate Professor in the Department of Family and Community Medicine (DFCM) and University Health Networks’s Chief of Family Medicine, explains. “On December 30 we were asked to develop a strategy to get vaccinations into long-term care homes. 24 hours later, we visited our first home and invited other primary care leaders to shadow our mobile vaccination teams and share the same model across the city.”
“We’re sharing logistics and resources to get residents vaccinated as quickly as possible. There are no silos here, everyone has put down their hospital tags and come together as Team Vaccine. The ability to become one team so quickly has been very moving and we want this to be the model for the future, pulling in the same direction to protect those that need it most.”
At each home, previously hesitant staff and residents see colleagues and friends getting their shots and ask to be vaccinated.
“In the Toronto East region we visited all our 22 long-term care and retirement homes in four days, safely vaccinating 2500+ eligible residents and staff by Jan 6, 2021. The level of collaboration and organization between hospitals, logistics and homes was incredible. The homes had the consents ready, and on Dec 31 it took just five minutes to fill our shifts with six teams of volunteers going out each day," explains Dr. Tia Pham, Associate Professor in the DFCM and founding director of the East Toronto Family Practice Network. “But what is most meaningful is the overwhelming and ecstatic response by residents and families, who sometimes watch the moment on the phone. Receiving the vaccine is a huge relief. The big smiles, grateful tears and beautiful words shared with each of us while vaccinating is a real gift.”
The scale and speed of vaccination in long-term care facilities is a testament to the passion and impact of DFCM faculty and primary care teams.
“The collaboration and team-work on display across DFCM and Toronto’s hospital networks has been truly inspiring”, says Dr. David Tannenbaum, Interim Chair in DFCM. “Throughout the city, family doctors and other primary care providers are showing strength, resilience and determination, and doing remarkable work to protect our most vulnerable residents and those who care for them.”
Now, #TeamVaccine is moving to residential homes and partnering with regional hospitals to vaccinate more Ontarians. With leadership from Dr. David Kaplan, Associate Professor in DFCM and Chief of Clinical Quality at Ontario Health, Lemieux, Pham, and other family physician leaders across Toronto, primary care teams are leading this unprecedented COVID-19 vaccination program.
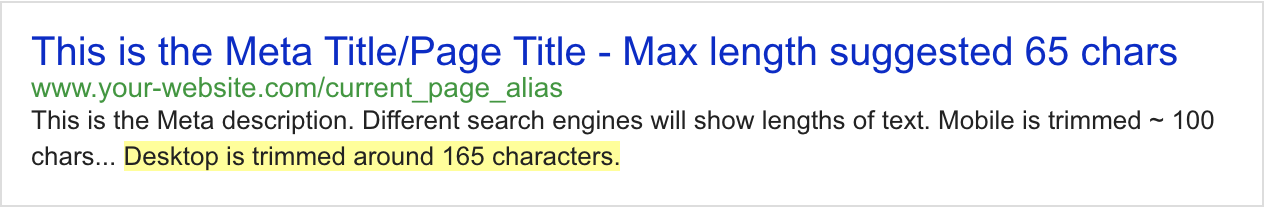
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

How to Incorporate Virtual Supervision of Learners into Medical Care 2.0
Google map
This seminar builds on previous versions and utilizes the collective virtual supervision experience/inexperience of Faculty, Residents and Medical Students. There will be several short practical demonstrations and lots of opportunities to ask questions. The seminar is accredited for 2 hours Mainpro+.
The seminar will include:
- How to prepare, supervise and debrief with learners providing virtual care.
- Demonstrations of phone and video supervision.
- Time to talk with Faculty and Learners to share tips/tricks.
- Key resources to support virtual supervision.
Please register at: https://zoom.us/meeting/register/tJUrfuChrzkiG9yaUjOXMgsas5wd-Gc6o4Ze
For those who are unable to attend, there are many resources on our DFCM COVID-19 Resource page under the “Educational Resources for Faculty & Residents” to assist you with virtual supervision and teaching.
Please note that a similar session for FMLE and Electives/Selectives preceptors will be held on November 11th. This session will also include program specific updates. These teachers are welcome to attend on whichever date best suits their schedule.
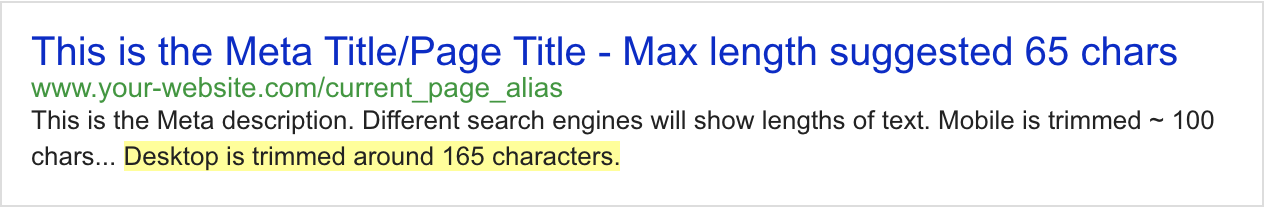
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Experiential Simulation Highlights Plight of Low-Income Canadians
Walking a mile in someone else’s shoes takes on another meaning in “Stand Up for Health,” an experiential learning simulation that shows physicians and medical students the challenges faced by economically vulnerable Canadians.
Over 800 people have participated in the two-hour workshop, which simulates the life of low-income Canadians with a focus on the social determinants of health.
“The intent of this simulation is to develop empathy among participants by connecting the concrete experiences of people living with low incomes and the emotions that arise from their challenges, and coupling this with a reflective process,” says Latif Murji, a second-year resident in University of Toronto’s Department of Family and Community Medicine (DFCM) and St. Michael’s Hospital who created the program. “Every moment where emotions are evoked, we inject real Canadian statistics and facts which provide context to the experience.”
The simulation includes issues such as food insecurity, the costs associated with caregiving and how gender and race can affect one’s experience in society. Critical questions are peppered in the experience: ‘You were in a rush this morning and forgot your lunch, a smartphone app says, ‘Do you go for the fast food lunch for $5 or do you go to the healthier salad bar, costing $10?’
“What seems like a simple answer to most of us is quite complicated for a person who is receiving a low income,” says Latif. “We have members of our society that cannot afford the healthy choice, because it is often the more expensive option.”
The simulation ends with small-group discussions that highlight various social determinants of health. Participants have the opportunity to reflect on their own socio-economic status in comparison to the roles they had been immersed in. Many acknowledge that the simulation has forced them to reexamine some aspects of their own lives.
“I’ve had participants say that they found Stand Up for Health really eye-opening because in addition to facing unique experiences that they haven’t previously encountered, they also found familiar decisions challenging because their socio-economic context is totally different. Not only do they experience living with a low income, but other members of society can perceive them differently because of their gender or race.”
Dr. Katherine Rouleau, Director of Global Health Program at DFCM, participated in the Stand Up for Health simulation at the Global Health, Family Medicine and Primary Care Conference in January 2017. It is an experience that she called ‘transformative’.
“The unique aspect of Stand Up for Health is that it connects knowledge with emotion, which is key to an experiential simulation. You’re forced to decide between challenging alternatives,” says Dr. Rouleau. “It can leave you shaken. In our world of disposable experiences, this simulation does not let you quite dispose of it. The experience ends with a group debrief. While it is not always comfortable, it is a cool way to learn and it leaves you with something to revisit later on.”
Latif started Stand Up for Health in the summer of 2012 before he began medical school at University of Toronto. He used many of his personal experiences growing up in Scarborough to develop some of the foundational aspects of the simulation. His first participants were at-risk youth in Scarborough who already had exposure to several elements of the simulation. Stand Up for Health at the time was used, in part, to empower and inspire youth to pursue higher education, while it is now used more broadly in medical education to teach the social determinants of health and develop empathy in participants.
For now, Latif is rolling out the simulation to medical students, residents and faculty but his goal is to encourage more people outside of the medical realm to understand the social determinants of health by walking in another person’s shoes and sparking discussions on public policy and health equity.
Related item
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Watch a Video Q&A with Dr. Michael Kidd, DFCM Chair
DFCM welcomed its new Chair, Dr. Michael Kidd, on May 1st. Dr. Kidd has over 30 years’ experience as a family doctor, primary care researcher and medical educator, with special interests in the primary care management of HIV and viral hepatitis, mental health and Indigenous health. He is a medical graduate from The University of Melbourne, and has a doctorate in medical education research from Monash University. His academic experience includes eight years as the Dean of the Faculty of Medicine, Nursing and Health Sciences at Flinders University in Australia, and 13 years as Professor and Chair of the Department of General Practice at The University of Sydney.
Dr. Kidd recently completed a three-year term as President of the World Organization of Family Doctors (WONCA), a global professional organization in formal collaboration with the World Health Organization (WHO) and representing over 500,000 family doctors in over 150 countries. His global health experience includes service as a consultant to health ministries in many countries, as well as with the WHO, the United Nations Program on HIV/AIDS (UNAIDS), and the Primary Health Care Performance Initiative of the WHO, World Bank, and Bill and Melinda Gates Foundation.
Dr. Kidd has served two terms as the elected President of the Royal Australian College of General Practitioners, and he is an elected Fellow of the Australian Academy of Health and Medical Sciences. He has served as a member of numerous Australian Government advisory committees and boards, including the National Health and Medical Research Council, and has served as a director of several national and international health and medical organisations, including Australia’s national mental health initiative, beyondblue. He has been involved in many voluntary community activities including leading the medical team for the gymnastics and basketball venue at the Sydney Olympic Games in 2000, and being a regular health commentator on Australia’s national youth radio station, JJJ, appearing as “Medical Michael”. In 2009, in the Queen’s Birthday Honours List, he was made a Member of the Order of Australia for his services to health care and education.
Get to know him better through a short Q&A below, where he answers questions about his background in academic family medicine, his motivation to join the DFCM, and his ideas about the future of family medicine in Canada and around the world.
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Celebrating DFCM's Senior Promotions: Full and Associate Professors
Nine faculty members from the Department of Family and Community Medicine have been promoted to the rank of Associate Professor and one to the rank of full Professor.
This reflects the exceptional contributions these individuals have made to our Department. Thank you to each faculty member for your hard work in promoting education and scholarship within our University, as well as nationally and internationally. I look forward to learning more about this great work.
Below are highlights of just some of their many accomplishments.
Thank you,
Dr. Michael Kidd
Chair, Family & Community Medicine, University of Toronto
Professor
Dr. Mike EvansDr. Mike Evans has taken a truly innovative path, focused on developing evidence-based health media that is engaging and infectious for the public. Throughout, he has endeavoured to find the best evidence to improve health and then used progressively more interesting media to communicate with his expanding audiences. His work is pioneering: he has extended the use of social media for health information in such a way that other researchers are following suit in using the techniques he has developed, such as his YouTube videos and other modalities. Dr. Evans has led the way as an innovator and entrepreneur who has devoted himself to developing and implementing novel approaches to patient education and systems transformation. | |
Associate Professor | |
 | Dr. Gary BlochDr. Bloch's work focuses on developing novel ways for physicians and other health providers to have an impact on their patients' social vulnerability. Dr. Bloch’s major contribution has been the development of the Clinical Tool on Poverty for Primary Care: a simple three-step approach to addressing poverty in a typical family medicine office setting. Dr. Bloch is also recognized for exemplary professional practice in developing approaches for addressing the social determinants of health. Dr. Bloch’s work lies at the intersection of family medical practice, public health and social policy, and his dedication to improving the health of the most marginalized citizens. |
 | Dr. Sharon DombDr. Domb focuses on enhancing the integration of technology into practice with the twin goals of improving patient care and educating current and future physicians. In the clinical realm, she has contributed significantly to obstetrical care and education. She has gained national and international stature in bridging the gap between Information Technology (IT) systems and patient care, with a focus on its application in primary care. Her scholarly activities address topics of critical importance to family physicians and include education with an emphasis on maternity care and the use of health information technology. |
 | Dr. Curtis HandfordDr. Handford's focus - supported by his research and expressed by his teaching and education - is on the exploration of generalism and its expression in 21st century clinical practice. He has embedded the theory and principles of generalism in developing standards of practice in specific areas such as management of people with HIV and addictions. Dr. Handford is recognized as a leader in education. He was appointed the inaugural program director for the Masters in Community Health, Family Medicine in the Dalla Lana School of Public Health at the University of Toronto, in 2010. |

| Dr. Fok-Han LeungDr. Leung's work has focused on developing innovative educational programs, materials and tools. As the Associate Course Director of Community, Population and Public Health (CPPH), a course in the first two years of the MD Program, Dr. Leung introduced innovations for both students and faculty and has developed resident assessment and evaluation tools. |
Dr. Danielle MartinDr. Martin is well-known for her research and policy work on publicly-funded health care, with particular emphasis on access for vulnerable populations. An important aspect of her expertise is evidence-based knowledge translation to policy makers and the general public. Dr. Martin’s work in this area has been sustained, impactful, and recognized at U of T, nationally and internationally. Dr. Martin has emerged as a powerful national leader in healthcare policy and health system improvement. | |
 | Dr. John MaxtedDr. Maxted’s focus is on improving patient safety in the primary care setting, a realm that until recently was neglected in comparison to hospital-based and specialist care. Dr. Maxted has been a champion of developing and introducing practical, applicable approaches to the primary care setting. His approach has been a collaborative one, working with organizations to develop standards and promote their uptake in practice. |
 | Dr. Alan MonavvariIn 2014, Dr. Monavvari was selected as Chief of Family Medicine at Markham Stouffville Hospital, a community-affiliated academic site. Dr. Monavvari has made a significant impact through excellence in CPA and teaching, especially on the continuing education of physicians with the development and dissemination of a wide variety of high quality programs nationally. Dr. Monavvari has shown a strong commitment to education and teaching of students throughout the continuum of medical education and has been very involved in recruitment, selection and education of IMGs since 2008.
|
 | Dr. Susan Glover TakahashiDr. Glover Takahashi focuses on two broad areas in postgraduate medical education: curricular innovations and competency-based medical education practices. She has made significant contributions to evolutionary changes in CanMEDS. Dr. Glover Takahashi is an internationally recognized leader in medical education in several fields, including competency-based medical education, postgraduate medical education program accreditation, assisting residents in difficulty, and curriculum development related to health professional field education. |
 | Dr. Karen WeymanDr. Weyman's clinical work is in the Family and Community Medicine Academic Unit at St. Michael’s Hospital, where she became Department Chief in 2015.Building on her work with homeless youth and youth at risk, Dr. Weyman developed an advocacy experience and elective which is now mandatory for all third-year students. Dr. Weyman has also been extensively involved as curriculum development lead in the innovative Longitudinal Integrated Clerkship for third year medical students at the University of Toronto. |
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Motivating women in rural Uganda to participate in prenatal care
In Uganda, located in East-Africa, where approximately 6000 women will die annually due to pregnancy-related complications, providing access to and encouraging women to use prenatal care provided by trained medical professionals is a major priority for the country.
 Many of these deaths occur in rural areas, where access to prenatal health care is challenging due to isolation, a lack of education around the utility and availability of prenatal care, and an inclination to use traditional healers rather than go to professional service providers.
Many of these deaths occur in rural areas, where access to prenatal health care is challenging due to isolation, a lack of education around the utility and availability of prenatal care, and an inclination to use traditional healers rather than go to professional service providers.
A new study by Department of Family and Community Medicine researcher, Dr. William Cherniak and his colleagues is proving the power of images: by advertising on Uganda radio that women will receive free ultrasounds, and thus the opportunity to see their unborn baby in the womb, while visiting prenatal care clinics, visits to prenatal clinics grew in some cases six-fold. The results of the study are now published in an open access format online in PLOS ONE in their Maternal Health Task Force Series, supported by the Bill and Melinda Gates Foundation.
“Some areas of Uganda also have the highest rates of mother-to-child HIV transmission in the world so the original thought was that if we can get women to go to maternal health clinics to receive treatment to reduce the risk of HIV transmission, we could also provide them with basic prenatal care,” explains Cherniak, also an emergency physician at Markham Stouffville Hospital. “But it evolved from there: why focus just on HIV positive pregnant women when so many women suffer pregnancy complications that can be identified and potentially prevented if they receive quality prenatal care?”
Ultrasounds in particular are necessary in helping healthcare workers identify potential complications, such as a multiple pregnancy, low-lying placenta, whether a baby is breech and other issues.
Cherniak teamed up with an Infectious Disease Specialist at Western University, Dr. Michael Silverman and a local Ugandan physician, Dr. Geoffrey Anguyo and his non-profit organization Kigezi Healthcare Foundation (KIHEFO) to conduct a randomised cluster-controlled trial across eight areas of rural Uganda to determine the effectiveness of advertising ultrasounds. In four communities the maternal care clinics were advertised on the radio without mention of the ultrasounds (although all of the women were offered an ultrasound free of charge after arriving at the clinic); whereas in the remaining four communities, the radio advertisements emphasized the ultrasounds and the opportunity for women to see and receive a photo of their unborn babies.
“The response to the radio ad that marketed the ultrasound was really amazing- our rate of attendance grew significantly, including by women with who had previously seen a traditional healer for their care,” says Cherniak. “The women who attended the clinics were overwhelmingly positive about their experience; there were big smiles all around when they saw their babies- even by those who were skeptical or unsure of the ultrasounds at first.”
The ultrasounds are conducted by ultrasound technicians in Uganda who are trained both to conduct the ultrasound and diagnose and share the results.
Since part of the grant Cherniak and his team received was used to purchase portable ultrasound machines, the machines were left in Uganda and continue to be used in rural Ugandan communities by KIHEFO since the study began in 2014. Cherniak and the non-profit organization he cofounded, Bridge to Health and their partners in Uganda are now examining ways to expand the project and provide more portable ultrasound machines across the country through grant opportunities with Grand Challenges Canada and sponsors around the Greater Toronto Area, including Rotary Clubs, Lebovic Enterprises and TACC Construction Ltd.
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

15th Annual Education Achievement Celebration
Google map
RECEPTION: Friday, May 5, 2017 - 17:30 - 19:30
Every year, the Council of the Education Vice-Deans has the pleasure of hosting the Education Achievement Celebration, a Faculty-wide event to recognize and celebrate the tremendous contributions being made to medical teaching and education scholarship throughout the Faculty of Medicine.
Our 15th Annual Education Achievement Celebration will be held in the Great Hall at Hart House on Monday, May 15, 2017. Please save the date. Doors will open at 5:00 pm. The event itself will get underway at approximately 5:30 PM.
In domains across the education continuum, our faculty, learners and staff have a significant impact on medical education. From undergraduate medical education to faculty development, our collective commitment to fostering and inspiring educational excellence is clear – it is reflected in the strength of our programs and departments and in the calibre and achievements of our community.
LOCATION
The Great Hall, Hart House
7 Hart House Cir.
Toronto
M5S 3H3
CONTACT: Office of the Education Vice-Deans: medicine.awards@utoronto.ca
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Toronto International Program: Strengthening Family Medicine and Primary Care
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.




Due to the COVID-19 pandemic, we will not be offering the in-person TIP-FM in 2021. We are excited to announce the V-TIPS program, a virtual edition of the TIP-FM program, which starts in April 2021. For more information, visit our V-TIPS page.
Program Description
Register for the Toronto International Program (TIP-FM) to learn about effective family medicine and the Canadian healthcare system from Canadian leaders, to network and learn from the experience of other like-minded family medicine champions from across the globe. The TIP-FM program is a course for leaders in the area of healthcare delivery, policy, and academia interested in strengthening family medicine and primary care. The goal of the program is to enhance leadership capacity in family medicine and primary care by building on lessons learned in the Canadian and global context.
The course gives an overview of the foundations and key elements of family medicine in Canada and combines that with a deeper exploration of specific elements of family medicine and primary care relevant to participant's local reality. The course is taught by faculty leaders from the Department of Family and Community Medicine (DFCM) and others at the University of Toronto - the largest family medicine training program in North America.
C0-TIPS
An example of continued mutual collaboration from the DFCM and international colleagues is the CO-TIPS virtual forum which was formed in response to the COVID-19 pandemic. CO-TIPS provides a space to examine and discuss key issues pertinent to the delivery of primary care in settings around the world. Since March 2020 TIPS graduates and DFCM Faculty have participated in these discussions which have provided a space for learning, reflection, wellness and scholarly activity.
Curriculum and Course Requirements
Course Requirements
All of the program components will be delivered in English. Translation will not be provided. Participants should be fluent in English.
Curriculum
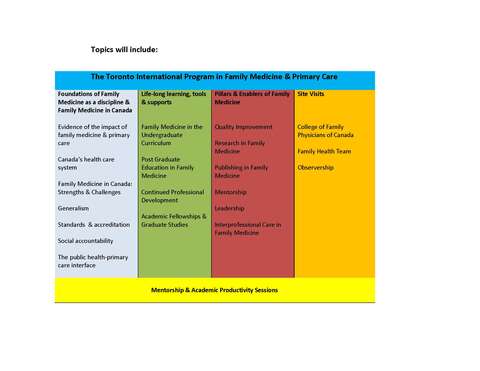
The course is customized to meet the participants' identified learning needs and will include:
- Presentations by Canadian leaders in family medicine
- Workshops on policy, research, quality improvement, and healthcare delivery
- Small group interactive discussions
- Customized, self-directed learning with experts in primary care and family medicine
- Visits to community health centres, family medicine clinics, hospitals, and the College of Family Physicians of Canada
- Clinical observership opportunities
- Resident supervision observership
- Networking with leaders and colleagues from around the world
Course Objectives
By the end of the program participants will be able to:
- Describe the evolution and challenges related to the development of family medicine in various settings around the world.
- Reflect on key policy, health system and training features to strengthening family medicine.
- Describe the challenges and critical next steps in developing family medicine in local contexts.
- Have the opportunity to produce either a quality improvement plan, a strategic plan to address a critical issue in the development of family medicine, or an academic paper on your work in family medicine and/or primary care.
Registration Information
Registration Registration is now open.
Registration deadline: May 15, 2020
For more information contact dfcm.ghevents@utoronto.ca.
There are a limited number of partial scholarships available for individuals from low and middle income countries to help off set the cost of tuition. Please contact us for more information.
Faculty and Staff Travel 30,000 km Across Ontario to Support Rural Preceptors and Residents
When thinking about family medicine at U of T, DFCM’s affiliated teaching hospital sites in and around the Greater Toronto Area often first come to mind; yet DFCM includes over 30 community-based teaching sites throughout rural Ontario that make up its rural residency and teaching practices programs.
There are several ways family medicine residents at DFCM can gain experience practicing in rural communities. The Teaching Practices program provides a two-month rural placement as part of the PGY2 year in the Family Medicine curriculum, where they are exposed to the opportunities, challenges and rewards or practicing in rural communities. Or residents can choose to enrol in the Rural Residency Stream which allows them to spend the entire second-year of their family medicine training in Midland, Orillia, Port Perry or Orangeville.
Supporting and engaging rural preceptors is challenging: they are distributed at sites from as far east as Kincardine, as far west as Campbellford and as far north as Red Lake (about a 6 hour drive from Thunder Bay).
That’s why Dr. Erika Catford, Director of the Teaching Practices Program, Dr. Gwen Sampson, the professional development representative for Teaching Practices, and Fadia Bravo, the Teaching Practices Program Assistant, headed out on a two-week, 30,000 km faculty development tour that included conducting workshops for 95 preceptors in 22 communities.
Faculty at each site had an opportunity to select from a list of seven accredited MainProC Practice Based Small Group (PBSG) learning modules. The workshops were selected based on their needs, including topics like providing feedback to learners, interprofessional education and collaboration and time efficient teaching strategies. During the visit, preceptors were also able to update their practice profile.
“We’ve conducted many efforts to engage with our rural preceptors online, however, we have found that face-to-face visits have so many long-term benefits that the travel is worth it,” says Dr. Sampson, who also practices in Stouffville.
This isn’t the first time a tour of this nature has been undertaken: in 2012 they visited over 23 rural sites to create a video profile of each practice and community. These videos are used to provide residents with the opportunity to review and make the best decision before selecting their choices for the Teaching Practices matching process.
The videos can be viewed on DFCM’s YouTube site.
Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.
Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.